A device that could save the lives of women all over the world by treating postpartum haemorrhage (PPH) has received significant funding, and could be available widely soon.
The University of Liverpool in the UK has been awarded £850,000 from the National Institute for Health Research (NIHR) to further develop the device, which could have a major global impact on the rate of maternal deaths.
Professor of International Maternal Health, Andrew Weeks from the Institute of Translational Medicine received the funds from NIHR's Innovation for Innovation programme for the PPH Butterfly.
PPH is often defined as the loss of more than 500ml or 1,000ml of blood within the first 24 hours following childbirth. It is a common maternity emergency affecting 40,000 British women each year. Although it can usually be treated in the UK, many suffer long-lasting complications.
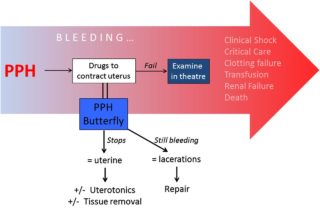
Globally PPH remains a major cause of death and is responsible for around 25% of the 289,000 maternal deaths annually. Although common, its management has changed little over the last 30 years. The new device, the PPH Butterfly, works to not only stop the bleeding immediately, but also help diagnose its source.
The most common cause of PPH is an inability of the uterus to contract adequately after childbirth. Typically it is treated with bimanual compression (BMC), where one hand is placed within the vagina and the other hand is on the abdominal wall to compress the uterus. This is effective, but very uncomfortable for the woman, said the researchers.
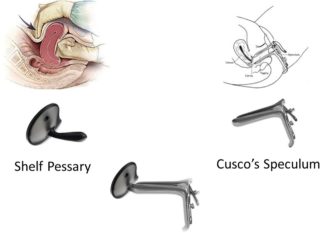
“We designed a device that could replicate BMC without inserting a hand vaginally, therefore being less invasive. It could also help in diagnosing the source of the bleeding.”
The first clinical trials of the device have now been successfully completed. The next phase will see the device tested this summer on women identified as suffering from PPH. “It is designed to be easy to use and low-cost and allows for smooth insertion and removal. It is acceptable to clinicians and consumers and performs well in tests,” added the researchers.
“This funding is vital in helping us to take the development of this device forward. It is also a testament to strong partnership working with the University, the NHS and Industry partners,” said Professor Weeks, who is also a consultant obstetrician at the Liverpool Women's Hospital.
“Going forward we are currently developing a training package for those who will be using it with view to the clinical trials this summer.”
Read the study here: http://innovations.bmj.com/content/early/2017/01/30/bmjinnov-2016-000144